
Medical validation: June 27, 2014dr Jesus Cardenasallergologist
Mastodynia is united or bilateral breast pain.It is a frequent symptom, but which should be considered seriously, and to treat systematically: it is often the clinical manifestation of a crippling imbalance, whose treatment is necessary, in the short term to relieve the patient, and in the longer term to avoid or delay the development of benign mastopathy, which is currently believed to be a risk factor for breast cancer.
- Breast pain: Physiological reminder
- Variations during the menstrual cycle
- Diagnosis of mastodynia
- Isolated mastodynia of the girl
- The mastose mastodynie of the woman of the forties
- A special case: mastodynia and hormonal contraception
Breast pain: Physiological reminder
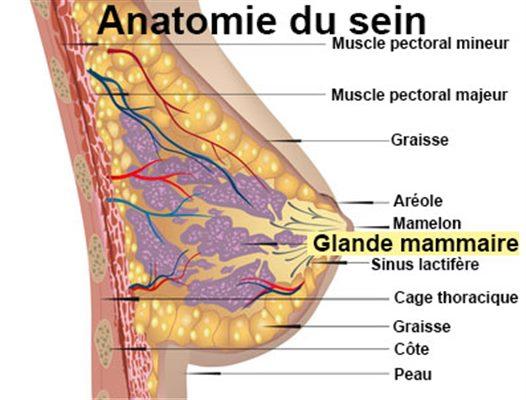
On the histological level, the breast is made up of three compartments: epithelial (galactophores and acini channels, with myoepithelial elements), connective (support fabric) and adipose.The relationship between these different tissues varies according to the individual constitution, the age and the physiological state.
On the physiological level, breast life is closely under hormonal dependence.
Estrogens have two main effects:
The main action of progesterone is to modulate or inhibit the effects of estrogens:
Other hormones are involved in breast physiology even if their exact role is still misunderstood;This is particularly the case with insulin, cortisol, growth hormone and thyroid hormones.
The breast action of circulating hormones is modulated by the existence of receptors, both in the glandular epithelium but also in fibroblasts and the conjunctive tissue, the best known being the receptors with sex steroids.The concentration of receptors is linked to cell richness and is reduced in case of fibrosis;It also varies during the menstrual cycle, in a comparable way to its evolution in the endometrium.Prolactin has an essential role in the acquisition of these hormonal receptors, which would be likely to explain the protective role of lactation towards the risk of breast cancer.
Finally, there seems to be independent local self -recorded and paraccrine mechanisms responsible for real in situ steroidogenesis from the sulfatasic and aromatasic estrone activities.These local mechanisms are likely to modify the response to circulating steroids;We thus understand the diversity of clinical tables made, as well as the randomness of the therapeutic response to the various hormones administered.
Variations during the menstrual cycle
Hormonal breast stimulation varies during the menstrual cycle:
We therefore understand the possibility of mastodynia by congestive phenomenon, from a simple hormonal imbalance at the expense of progesterone: "hyperfolliculinie" relative, or rather luteal insufficiency of the yellow in general itself itself to a central disturbance of the secretionGonadotrophins.You should know that the crippling imbalance can be discreet, only express themselves at the mammary tissue and be elusive by the dosages of estradiol and plasma progesterone.
À voir aussiDossierMuscle aches
ArticleBreast reconstruction: panorama of different techniques
The repetition of normal cyclic phenomena determines in the long run the fibroadip involution and the senescence of the breast by progressive decrease in the glandular tissue.On the other hand, the cyclical repetition of pathological phenomena as an ESTRO -rogestative imbalance determines a dystrophic senescence which opens the door to benign or mastoses mastopathies.These are extremely variable and can relate to the three compartments:
These few notions make it possible to understand the privileged role of progesteronotherapy in the treatment of mastodynia, the prevention of mastopathies and, to a certain extent, the prevention of breast cancer.A patient carrying benign mastopathy has a risk 3 to 4 times higher than another to develop breast cancer.
Finally, we must not ignore the role of a particular psychoexistial terrain in the occurrence and the evolution of this breast pathology, so much so that for some, it is a real psychosomatic disease.The role of psycho-affective events is well known, and it is likely that mastodynia is only reflected at the breast level a cripproggogestative imbalance linked to a psychogenic dysovulation.Conversely, the discomfort of breast pain and an element of cancerophobia do not fail to sound in the long run on the psychological level.
Annonce sponsoriséeVous venez d'apprendre votre cancer ? Demandez un 2ème avis en ligne auprès d'un expert de CancerConsult. Plateforme de 2ème avis en ligne en 7 jours avec plus de 40 Experts référents Français dans leur pathologie.ConsulterDiagnosis of mastodynia
The diagnosis of mastodynia is easy to install: united or bilateral breast pain, a localized tension or burning type, which is quite easily different from parietal pain, especially when their occurrence is cyclic, as is generally the case.
As in most subjective syndromes, the problem is to know from when a banal premenstrual breast tension becomes a pathological mastodynia that it is necessary to treat and monitor.
This is the side-hustle I started: https://t.co/zTiYonquua 6 months later it pays ALL my bills. * No experience r… https://t.co/MPG4HCt94e
— The Giver 💰 Mon Jun 21 17:57:23 +0000 2021
Isolated mastodynia of the girl
Mammary pain in general bilateral, with irradiations (back, internal side of the arm) as a function of the development of the chest, occurring in premenstrual and sometimes preovulatory periods.
The interrogation goes in search of family history, it also specifies the regularity of cycles, the possible association of other premenstrual phenomena (weight gain) and the existence of other painful cyclical genital phenomena.The clinical examination can be practiced at different times of the cycle to assess the variability of objective phenomena;One of the examinations must in any case situate itself in the immediately postmenstrual period when the breast is relaxed, less warm and less sensitive.It must include the usual two times:
The examination cannot be complete without the exploration of axillary and supiclavicular hollows.
Treatment
In the case of isolated mastodynia, the examination is strictly normal and there is no clinically detectable abnormality in the breasts.It is then a question of relieving and installing surveillance in the longer term:
Therapy must be underpinned by clear information from the patient, who must be reassured about the nature of this cyclic pain and her hormonal character.
Adjuvant therapies are always welcome: analgesics and light anti-inflammatory drugs, vitamin A, veinotonics, even minor diuretic in the event of more general premenstrual edematous phenomena.The sedatives and all the more reason the various psychotropic drugs, the use of which may seem judicious, given the terrain, are rather to be avoided due to a possible indirect, even light mammotropic action (dysovulation or hypersecretion of prolactin).
It is in reality therapy by progesterone which is the most indicated, both for its immediate effects and for its preventive role of the transition to a mastosis.
The local application of progesterone gel must always be attempted at first, because it is effective and without systemic effect, some patients, however, are put off by this long -term practice.The use of synthesis of synthesis of synthesis close to progesterone (retroprogesterone, moves) in the second part of the cycle also gives excellent results and can be continued without inconvenience over long periods even in young patients.
Surveillance must also rely on broad information from the patient, who must regularly examine her breasts according to specific methods that have been taught to her, and know how to seek changes such as the appearance of a mass.Monitoring must also take into account high -risk factors of breast cancer.
The main risk factors for breast cancer
In these cases, the information of the young patient should not omit to report the "preventive" role of pregnancy and lactation.On the practical level, and apart from special cases, it seems sufficient to provide an annual clinical examination, even biennial for an isolated mastodynia.The hormonal dosages are useless.In case of isolated mastodynia of the girl, mammography is also useless (especially since the breasts are radiologically very dense), except when she is claimed by the patient, or that it is a woman torisk.
If this isolated mastodynia table can disappear spontaneously, as a result of a pregnancy for example, it represents more frequently the start mode of real mastopathy, to lead to the following table.
The mastose mastodynie of the woman of the forties
Mastodynia remains punctuated by the rules, but there are also more capricious manifestations: persistence of mastodynia for several weeks, or on the contrary disappearance of symptoms for a few months.This often irregular evolution during the year leads to cautiously interpreting the results of a therapy.The examination discovers the united or bilateral presence of nuclei or irregular mastose cupboards, of variable volume in time.The existence of common -looking adenopathies is not uncommon.A discharge of the nipple must always be sought.This painful mastopathy is readily associated with other manifestations of genital dysfunction: premenstrual syndrome predominantly egging or psychological, dysmenorrhea, pelvic pain ...
Additional examinations are essential here:
Treatment des mastodynies
Therapy still uses progesterone by installing if necessary a real escalation in the event of insufficient results: percutaneous progesterone, then synthesis progestoges close to progesterone, and in the event of failure, PS more powerful (Nor-Androstanes).The latter can be administered in high doses during the last ten days of the cycle.It is also possible to prescribe them for three weeks out of four.This type of treatment has an over -added contraceptive effect, but can however lead to atrophies of the endometrium and weight gain.
Apart from progesteronotherapy, other types of hormonal treatment have been proposed and constitute an appeal in specific situations:
The surveillance
The whole problem is dominated by the fear of breast cancer, for at least two reasons:
Repeat that it occurs 3 to 4 times more often on mastosic breasts;
It is all the more difficult to delect as the primary signs of neoplasia can be confused or masked by the clinical and radiological signs of the mastosis.
Monitoring must include:
Benign mastodynia and mastopathies disappear as a rule with the drying up of ovarian secretions to menopause.This disappearance is often preceded by aggravation during pre-menopause, due to almost constant existence at this time of the genital life of proven, more or less sustainable luteal insufficiency.It also happens that breast pathology persists and still presents some push after the final stop of the rules;Some women keep an endogenous but not negligible endogenous estrogen level for months, even years, after menopause.Be that as it may, we currently recommend continuing to monitor a mastopathy after menopause, unable to know whether we are if the post-menopausic breast cancer occurs with predilection in an old mastosics.
Consult an online online
Besoin d’un avis médical rapidement ? Prenez rendez-vous simplement avec un oncologue
Consulter ConsulterI accept that Doctissimo uses my navigation data, namely my redirection to a teleconsultation site with a health professional, only for audience measurement purposes *
If you refuse, you will be redirected to the Teleconsultation site without Doctissimo being aware of it.In addition, if you have refused the use of cookies for audience measurement through the cookie setting module, no audience measure will be made regardless of the choice you have expressed here.To find out more about the management of your personal data and to exercise your rights, you can consult our Personal Data Protection Politics.
Je refuse J’accepteA special case: mastodynia and hormonal contraception
The appearance of a mastodynia under pill proves that the compound in question is responsible for a crumbling imbalance at the breast level for the patient considered;This is not a peremptory argument to put an end to hormonal contraception.On the other hand, it is essential to change compounds, and the transition to a more marked progestin climate generally makes mastodynia disappear.The maintenance of a compound responsible for a mastodynia appears particularly not recommended, taking into account the current physiopathological notions;Experience also shows that mastodynia is one of the most dissuasive manifestations for patients vis-à-vis the pursuit of cripprogestatives.
Given their perfect tolerance on the other plans, mastodynia constitutes with the disturbances of the cycle, the most rated side effects with the ESTROGGESTIVES weakly dosed.On the other hand, contraception by microdosed progestins, achieving real continuous progesteronotherapy, could appear as a real prevention of mastopathies;In reality, due to a less complete hypothalamo-hypophyseal inhibition, this type of treatment lets persist an estrogenic ovarian activity likely to cause an endogenous cripproggogestative imbalance.
Annonce sponsoriséeVous venez d'apprendre votre cancer ? Demandez un 2ème avis en ligne auprès d'un expert de CancerConsult. Plateforme de 2ème avis en ligne en 7 jours avec plus de 40 Experts référents Français dans leur pathologie.ConsulterIn summary, the pathophysiology of mastodynia with or without mastopathy appears unequivocal, and their therapeutics is centered on progesterone.The essential problem, in this patient who fears breast cancer and who indeed presents a risk greater than the average, is undoubtedly to acquire her active collaboration.We will never repeat enough that early clinical detection is generally due to the patient who is watching and examining herself regularly.The practitioner has a capital role in information and support for this level;It is also he who, in accordance with the personality of his patient, will best face the two usual difficulties: avoid unnecessarily multiplying explorations in a worried patient, and on the contrary, knowing how to bring her without worryA complementary exploration of which the time has come.
Slideshow: breast cancer: the most beautiful pink October campaigns







